I still remember the first time I noticed something wasn’t quite right with my vision. Straight lines seemed a little wavy, reading small print took more effort, and faces didn’t look as sharp as they once did. At first, I blamed tired eyes, more screen time, or just “one of those days”. But over time, that subtle discomfort turned into concern. That’s when I first heard the term ‘age related macular degeneration’, or AMD.
If you’ve come across AMD recently—through a doctor’s visit, a family member, or your own online search—you’re not alone. AMD is one of the most common eye conditions affecting people as they age, yet it’s also one of the most misunderstood. This article is my attempt to explain AMD in a simple, relatable way, from a user’s point of view—without medical jargon, fear, or confusion.
What Exactly Is AMD?
To understand AMD, it helps to first understand a small but powerful part of your eye: the macula.
The macula sits at the centre of the retina and is responsible for clear, detailed, straight-ahead vision. It helps us read, recognise faces, drive, watch TV, and do all the fine-detail tasks we often take for granted.
Age-Related Macular degeneration is a condition where the macula slowly gets damaged over time. The result? Central vision becomes blurry, distorted, or dark, while side (peripheral) vision usually remains normal.
One important thing to know right away:
AMD does not cause complete blindness.
But it can significantly affect quality of life if not understood and managed early.
Why AMD Feels So Scary at First
When I first learnt about AMD, the word “degeneration” really hit me. It sounded final. Irreversible. Like a steady downhill journey.
But the truth is more balanced.
AMD is progressive, yes—but it’s also manageable, especially when detected early. Many people with AMD continue to live full, independent lives for decades with the right care, awareness, and lifestyle choices.
Usually, fear stems from not knowing what to anticipate. Once you understand AMD better, that fear starts to loosen its grip.
The Two Main Types of AMD
AMD generally shows up in two forms:
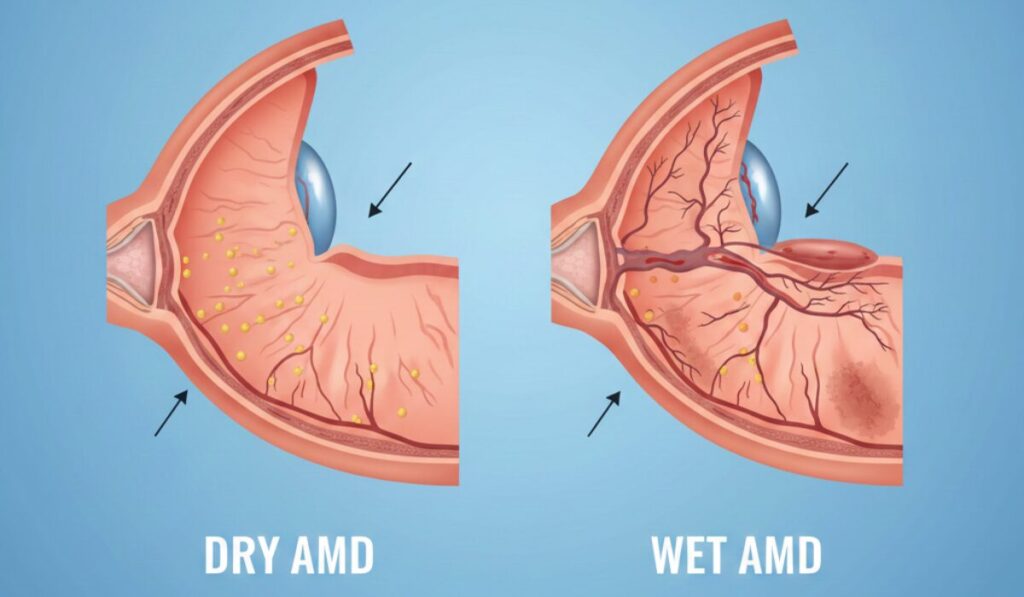
Dry AMD (More Common, Slower)
This is the most common type. It happens when the macula slowly thins with age. Tiny yellow deposits called drusen may appear, which doctors can see during an eye exam.
- Progresses slowly
- Vision changes are gradual
- Often manageable with lifestyle changes and monitoring
Many people live for years with dry AMD and maintain useful vision.
Wet AMD (Less Common, Faster)
When aberrant blood vessels form behind the retina and leak blood or fluid, wet AMD results.
- Progresses faster
- Can cause sudden vision distortion
- Needs prompt medical attention
While wet AMD sounds alarming, modern treatments have made a huge difference in slowing or stabilizing vision loss when caught early.
Common Signs People Often Ignore
One of the biggest lessons I learnt is how easy it is to dismiss early symptoms.
Here are some signs many people brush off at first:
- Blurry or fuzzy central vision
- Difficulty reading small print
- Straight lines looking wavy
- Trouble recognizing faces
- Needing brighter light to read
- A blank or black area in the middle of the field of vision
Because these changes often happen gradually, the brain adapts—and we delay action. That delay can matter.
Who Is at Risk?
AMD doesn’t appear overnight, and it’s rarely caused by just one thing. Risk factors include:
- Age (especially over 50)
- Family history
- Smoking
- Poor diet
- High blood pressure or heart disease
- Excessive sun exposure
- Long-term stress and poor sleep
What surprised me most is that many of these risks are within our control. That realisation alone makes AMD feel less helpless.
Living With AMD
One of the biggest myths about AMD is that life suddenly becomes normal again. That’s not true.
People with AMD continue to:
- Read (with proper lighting or aids)
- Use smartphones and tablets
- Work, travel, socialize
- Enjoy hobbies and family time
Small adjustments make a big difference—larger fonts, better lighting, contrast settings, and regular eye check-ups.
Technology, awareness, and early care have completely changed the AMD journey compared to even 20 years ago.
The Role of Mindset, Family, and Real Conversations
Health challenges don’t exist in isolation. They affect emotions, family dynamics, and self-image.
I’ve found that listening to real human stories—not just medical explanations—makes a huge difference. That’s why platforms focused on personal growth, reflection, and balance matter so much.
One such space I personally connect with is the YouTube channel New Age Indian Dad
Created by Rajesh Chotalia, the channel explores life as an Indian immigrant dad in America—balancing culture, family, identity, and personal growth. While it’s not a medical channel, the conversations around self-awareness, adaptation, and embracing change deeply resonate with anyone navigating life transitions, including health challenges like AMD.
Sometimes, understanding health isn’t just about eyes—it’s about mindset, acceptance, and learning to evolve without losing yourself.
The Role of Nutrition and Lifestyle

This part deserves special attention.
Over time, I realised that eye health is deeply connected to overall health. What we eat, how we move, and how we manage stress all play a role.
Helpful habits include:
- Eating leafy greens, colorful vegetables, and fruits
- Including healthy fats like nuts and seeds
- Staying physically active
- Protecting eyes from harsh sunlight
- Managing blood pressure and blood sugar
- Avoiding smoking
These changes don’t just help the eyes—they improve energy, mood, and long-term wellness.
Why Regular Eye Exams Are Non-Negotiable
If there’s one takeaway I’d underline twice, it’s this:
AMD can be present long before you notice symptoms.
Regular eye exams can detect early changes in the macula—even when vision still feels “fine”. Early detection opens the door to better outcomes and peace of mind.
Waiting for vision to worsen before acting is a gamble that’s simply not worth taking.
The Emotional Side of AMD
AMD doesn’t just affect eyesight—it affects confidence.
Simple moments like reading a menu, recognising someone across the room, or driving at night can suddenly feel stressful. That emotional weight is real, and it deserves acknowledgement.
What helps?
- Open conversations with family
- Asking for help without guilt
- Learning about assistive tools
- Focusing on what can be done, not just what’s changing
Acceptance doesn’t mean giving up. It means adapting with awareness and dignity.
Hope Is Very Much Part of the Story
The most encouraging thing about AMD today is progress.
Research, treatments, and awareness are improving every year. People are being diagnosed earlier, managing better, and living fuller lives despite AMD.
Understanding AMD transforms it from a frightening label into a condition you can live with, not live in fear of.
Final Thoughts
If you or someone you love is facing AMD, here’s what I’d say from personal reflection:
- Don’t panic
- Don’t ignore early signs
- Don’t delay regular eye check-ups
- Do stay informed
- Do make lifestyle changes
- Do you believe in better outcomes?
Vision is precious—but so is peace of mind. With awareness, timely care, and a proactive approach, AMD becomes a journey of adaptation, not defeat.
FAQ’s
Can AMD affect one eye more than the other?
Yes. AMD often starts in one eye and may progress faster there, while the other eye remains relatively stable for some time. This difference can make vision changes harder to notice, as the stronger eye compensates.
Is AMD inherited from parents?
AMD can run in families. If close relatives have AMD, your risk may be higher. However, genetics alone doesn’t determine outcomes. Healthy lifestyle choices, regular eye exams, and early detection can significantly influence how the condition develops.
At what age should people start screening for AMD?
People should begin regular comprehensive eye exams around age 40, especially if they have risk factors. Screening becomes even more important after age 50, as early macular changes often appear before noticeable vision symptoms.
Can AMD be reversed once diagnosed?
Currently, AMD cannot be reversed. However, its progression can often be slowed or stabilised with proper care, timely treatment, and lifestyle changes. Early diagnosis plays a key role in preserving remaining vision for as long as possible.
Does screen time worsen AMD?
There is no strong evidence that screen use directly causes AMD. However, long screen hours can cause eye strain and discomfort. Taking regular breaks, using proper lighting, and maintaining overall eye health are important for comfort and prevention.
Can people with AMD still drive?
Many people with early or moderate AMD can continue driving safely, especially during the daytime. However, vision changes should be regularly evaluated. Night driving may become challenging, and decisions should always be guided by professional eye assessments.
Are vision supplements necessary for everyone with AMD?
Not everyone needs supplements. Specific eye supplements are usually recommended for certain stages of AMD. An eye care professional can determine whether supplements are appropriate based on eye examination findings and individual risk factors.

